Elderly Bed Sores
Elderly bed sores or pressure ulcers are uncomfortable wounds that are commonly associated with the elderly and ill people, who cannot get up – or at least much less frequently, and who need more assistance to do so.
Bed sores are most likely to form, if you have to spend a lot of your time sitting down in a chair or wheelchair. Or lying in a bed. They are caused by pressure on bony body parts, such as the heels, elbows, tailbone… which are not regularly moved or adjusted.
Bedsores – also called pressure sores – are easily preventable.
Because pressure injuries are notoriously difficult to treat, especially in the elderly, the emphasis has to be on its prevention rather than cure.
Only round-the-clock watchfulness and care can help prevent pressure ulcers in the elderly. A fit and healthy person is likely to move regularly. However, elderly people who are less able to move might need the help of their family members or carers to change positions.

Treatment for bedsores in elderly also consists primarily of consistent, daily care – moisturising/ protecting the skin, frequent position changing, and maintaining a wholesome diet.
If you help in the care of an elderly person – to wash or dress them, always take a few moments to check their skin, especially around bony areas.
if after all your best efforts you find sores forming, there are a few home remedies and doctor-ordered treatments that can help you heal the affected areas.
Elderly bed sores: What Are Bed Sores?
Bed sores are injuries on the skin and the layers under your skin usually caused by prolonged pressure on your skin from sitting or lying down for long periods.
They are also known as pressure sores or pressure ulcers.
You can develop pressure sores on any part of your body, but they are most common on the boniest parts of your body. These are usually your elbows, heels, hips and the base of your spine.
Bedsores/ pressure sores can also form on the buttocks, shoulder blades, the backs or sides of your knees, ankles and toes.
Why Does Elderly Get Bed Sores? Causes of Bed Sores
Bedsores are caused by prolonged exposure to a number of factors.
You are most likely to develop these sores if:
- You are over 70 and have problems with mobility and dehydration. Your skin will also be thinner, and will heal more slowly
- You are confined to a bed or a chair due to illness, surgery, paralysis or obesity
- Your skin is exposed to friction – the rubbing or moving of the skin
- You suffer from bowel or bladder incontinence, or high levels of perspiration
- You have a bad diet
- If you suffer from a condition that affects your blood supply, makes your skin more fragile or causes movement problems (diabetes, kidney or heart failure, multiple sclerosis (MS), Parkinson’s disease).
- If you suffer from poor mental health such as depression or mental illnesses such as schizophrenia as your diet and personal hygiene might be poor, and you might spend large parts of the day sitting or lying down
Elderly bed sores: Symptoms of Bed Sores
How Long Before Bed Sores Develop?
Bedsores will normally form gradually, but they sometimes form within a few hours. You can stay aware of developing bed sores by being aware of what their early symptoms look like.
The symptoms of Elderly bed sores include:
- Discoloured skin – pale skin will tend to form red patches while darker skin tones will develop purple or blue patches
- Discoloured patches of skin that do not turn white when pressed
- A patch of skin that feels warm, spongy or hard to the touch
- Itchiness in the affected area
- The affected area might feel painful or like a burning sensation
Skinsight.com show pictures of what different sores might look like on different skin tones. Do not follow the link if you are squeamish.
If you are not sure if what you have is a bedsore, you can ask a friend, family member or your carer to check the photographs against your affected area.
Here’s a quick video discussing Bedsores and your care:
Elderly bed sores – At Home Care for Your Pressure Injuries: Video
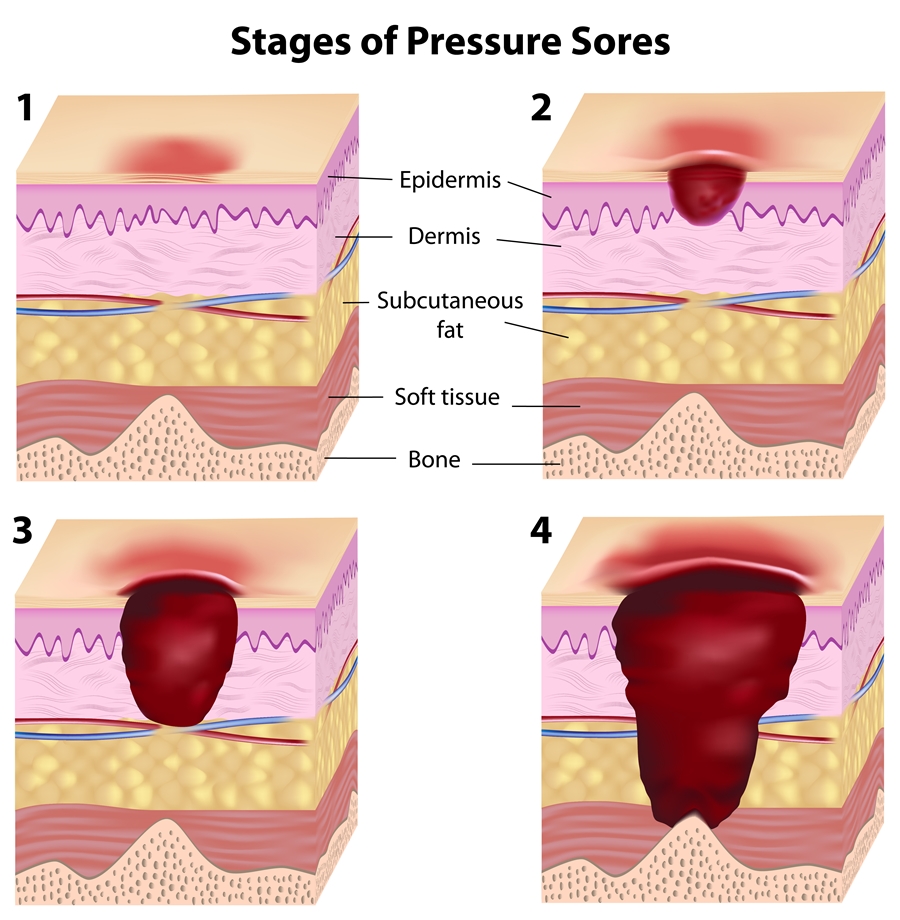
Elderly Bed Sore Stages/ Grading
Doctors and nurses give bedsores a grading between 1 and 4, depending on the level of severity. If your bedsores are not caught and treated at stage 1, then it most likely will progressively get worse.
The above symptoms make up Stage 1 of the bedsore stages.
- Stage 2 – your bedsore has become an open wound and might look like a pus-filled blister. The affected area will be red and sore and may be oozing clear fluid or pus.
- Stage 3 – your sore is now a deep wound that reaches deeper layers of your skin. It might look like a crater and have a bad smell. It will most likely be showing signs of infection: pus, redness and fever. There might even be black, dead skin around the sore.
- Stage 4 – your sore is even deeper and possibly reached your muscle or bone. You will have dead, black skin as well as signs of infection
As soon as you notice that you are developing bedsores, please alert your carer, nurse or doctor so that they can be treated as soon as possible.
The quicker you do this, the less likely it is for the sores to progress to one of the later stages.
Elderly Bed Sores Treatment: How to Treat Bed Sores in Elderly
The treatment for bed sores will be different, depending on what stage it’s at.
1. For all bed/ pressure sores, the first thing to do is to remove the source of pressure causing the sore to form. This might mean changing the position you are in when lying or sitting down, from one side to the other.
2. You might also find using a pressure-relief foam pad or cushion helpful.
3. If you are suffering from pressure sores, it can be useful to change your position every 2 hours if you are lying down. If you are sitting down, try some movement every 15-30 minutes.
4. You can also make a few changes to your diet to help hydrate your skin, if you are prone to pressure sores. Having a diet rich in protein, Vitamins A and C, as well as Zinc and Iron – and drinking plenty of water – could help prevent the sores from forming.
5. Clean the affected area with mild soap and water. Then dry gently. Doing these, you should notice a marked improvement in the Stage 1 pressure sore.
Stage 2 elderly bedsore treatment
This will start similar to Stage 1 – cleaning the affected area with water or a salt-water solution, then drying it gently. This might be sore as the skin is open now, so speak with your doctor or nurse about taking a painkiller 30 minutes or so before cleaning the affected area.
With a Stage 2 bed sore, you will want to cover it with a see-through dressing or moist gauze. If you notice any further sign of infection such as pus, redness or having a fever, then get back in touch with your doctor. This level of sore should heal between 3 days and 3 weeks.
Stage 3 elderly bedsore treatment
A Stage 3 bedsore will need a higher level of care so should always be treated by a doctor or nurse. They may need to remove any dead skin and will usually prescribe antibiotics for any infection. You might need to get a specialised pressure relief mattress to make sure you will not aggravate the sore even more.
Stage 4 elderly bedsore treatment: Do Stage 4 Bed Sores Heal?
If your pressure sore has spread to Stage 4, then you need to alert your doctor immediately.
Since this means you might start having infections in your muscles and bones, being able to treat it as quickly as possible is essential – so it doesn’t get worse.
A serious stage 4 bed sore may require surgery as a treatment option. During this surgery, your sore will be cleaned and closed up, possibly with the use of tissue from nearby healthy skin. After which the sore can take anywhere between 3 months and a year to heal.
As with all surgery, especially if you have bad health already, there are risks. Your doctor will talk you through these risks, and help you decide what the best treatment route is for you.
There are two other stages of pressure sores that your doctor might talk about. They might tell you that you have an ‘Unstageable’ bed sore. This means they cannot see the bottom of the bed sore, so they can’t tell how deep it is.
Your doctor will need to clean out the sore before they can tell what stage it is at. They might also say that the sore has caused Suspected Deep Tissue Injury (SDTI). This is how they describe a sore that looks like a stage 1 or 2 on the surface but is a stage 3 or 4 underneath the skin.
Elderly Bed Sores: Untreated Bed Sores
If you leave bedsore untreated, then it will only get worse. Eventually, it will move through the various stages, reaching Stage 4.
Stage 4 bed sores can be very serious and life-threatening – not only because one might need surgery to fix it, but it can also cause blood poisoning. This might occur if one also has a poor immune system, as is sometimes the case with a disability or advanced age.
Blood poisoning can lead to septic shock, where the organs start to fail. One will become cold, and the heart will beat faster. Blood poisoning, also known as septicaemia, needs immediate medical attention.
The sore might reach deeper levels of the skin, causing an infection. This is called cellulitis and can cause symptoms of pain, redness and puffing of the skin.
One will need a course of antibiotics to treat cellulitis. If the bedsores are on the lower back and spine, then it is even more complex and dangerous.
The sore can spread deep into the skin – to the bone – and spread to the membrane around the spine and brain, causing meningitis. If it reaches this stage, then one might be hospitalised and put on antibiotics as well as steroids.
Another danger with untreated bed sores is that it might also cause bone and joint infections – also called septic arthritis or osteomyelitis. These will need antibiotics to treat, and in the worst cases, you might need part of the bone or joint removed.
If bedsores become infected by certain bacteria, then one might have necrotising fasciitis which is a flesh-eating bacterium. If this happens, then you will need antibiotics and surgery to remove the dead skin that the bacteria have latched on to.
Many types of bacteria can affect and infect bedsores, such as clostridium bacteria that cause gas gangrene. These bacteria thrive in low-oxygen environments, and once formed, will release dangerous toxins.
These toxins cause pain and swelling in the affected area, and will need surgery as treatment. In the very worst cases, it can lead to the need to amputate the affected limb.
How to Prevent Bed Sores in Elderly
The best thing about bed sores is that it is mostly preventable. It is so essential to prevent the formation of bedsores in the elderly. And so much easier to stop early on.
If the early signs of injury are not noticed, they can worsen and become very painful or infected. Bedsores can do damage to the muscle or bone under the affected area of skin. And may lead to life-threatening complications such as blood poisoning and gangrene.
In the most severe cases, it may be unavoidable to amputate the affected body-part to stop the gangrene from spreading to the rest of the body.
Therefore, the smart way to stop this common problem is to prevent pressure sores and ulcers from forming in the first place. And working hard with your doctor/ nurse to stop them from becoming severe.
It can be challenging to prevent bed sores completely. However, here are some things you or your carer can do to reduce the risks:
Pressure Relief/ Repositioning
The most critical aspect in the prevention and treatment of pressure sores is certainly pressure relief. You absolutely need to avoid prolonged periods of pressure on any one area of your skin. You want to relieve pressure on areas that are vulnerable to damage – your heels, soles of the feet, tailbone, amongst others – by moving/ repositioning regularly.
It helps to time the intervals, say every 30-60 minutes. Some older adults may need more or less frequent repositioning than that, depending on your personal health status. So it’s equally important to work with your doctor/ nurse to determine the right timing for you.
Skin Hygiene
Daily attention to hygiene and dryness is necessary to keep the skin from becoming macerated. That is when the skin becomes soft, wet, or soggy to touch, due to being in contact with wetness/ moisture for too long. The skin will also look lighter in colour and be wrinkly. Maintaining skin hygiene also helps prevent infections.
The skin is a vital organ that serves to protect us from injury and infections. As we grow older, we begin to lose protective fat and muscle mass which thins the soft tissues between skin and bone.
Also, elderly people with cardiovascular conditions such as vascular dementia and diabetes, typically suffer from low blood supply. Both factors increase the elderly’s skin fragility to damage from moisture, shearing/ friction, and injury.
Skin hygiene involves the careful washing/ cleansing of your skin with non-perfumed, pH-balanced soap/ cleanser. Then pat your skin dry.
You also want to use a gentle moisturiser to keep your skin supple and prevent dryness.
Wetness on the skin increases the risks of pressure sores. If you live in a humid environment – or during hot/ humid weather – you may sweat more. To protect your skin from wetness, use a good barrier cream. Barrier creams are also useful, if you have bladder/ bowel incontinence.
Healthy Diet
Eating a healthy, balanced diet that contains a good variety of vitamins, proteins and minerals in sufficient amounts can help prevent bed sores. A healthy and varied diet rich in proteins, iron, zinc and vitamin C are the primary healing nutrients you want to enjoy, to speed up your healing process if you already have the pressure sores.
Your skin needs an adequate supply of fluid and nutrients to maintain its circulation and keep it supple. Supple skin is better able to withstand friction, and stay ulcer-free.
Supportive Devices
To reduce friction and shearing on elderly people’s skin, relevant manual handling techniques and supportive equipment/ devices need to be used.
Supportive devices help to improve and protect skin quality. They include products such as pressure-relieving cushions, mattresses, beds and chairs. These can be air-filled, genuine sheepskin or gel-filled.
Some pressure-relieving cushions have covers to keep your skin cool. If you tend to get hot and sweaty, you may prefer to use one of those.
Where necessary, you could use a pillow as a protective buffer between your skin and the bed/ chair to increase your comfort level.
With cushions and mattresses, you want them to be firm and supportive. Suppose a mattress or cushion is too thin or soft. In that case, it may become compressed, bringing your skin into contact with the surface underneath. That might consequently increase the risk of friction and skin shearing.
Skin shearing occurs when layers of skin are forced to slide over deeper tissues or one another. Such as when you slide down your chair/ bed.
Or when you slither back up your chair/ bed.
To reduce the risk of shearing, cushions and mattresses with individual balloon or egg-box-shaped surfaces; or foam mattresses and cushions with a cross-cut surface, are a good option. These types of cushions/ mattresses move with your body to reduce the pull on the outer skin layer.
If you are a carer to someone who is paralysed/ bed-bound, then equipment – such as a slide sheet or hoist – helps move your loved elderly one in and out of bed without damaging their skin.
Adequate Hydration
It is vital to ensure that you drink enough water to keep your body hydrated. Drink lots of water. Juices, tea, and milk also count in keeping your body adequately hydrated. Elderly people who become dehydrated often find that they cannot heal properly. It can be challenging to get into a routine of drinking water, but you must do it as a part of your daily health routine.
Avoid Smoking
Smoking reduces blood capillary circulation, near the surface of the skin.
If you smoke, it may be sensible to cut down on the quantity – or stop smoking altogether. That is because smoking can reduce the oxygen level in your blood, weaken your immune system and slow the healing rates. These factors increase the risk of developing bedsores.
Medication
Taking some medication such as steroids, cholesterol medications, antihistamines, and blood pressure pills etc. can cause the skin to dry out, significantly increase skin ulcers and slow down healing.
Elderly people who take these medications long-term are at an even higher risk of skin complications, because their skin is already fragile.
According to this research in the Journal of dermatology, “drug‐induced pressure ulcers (DIPU) are pressure ulcers caused by an external force {friction, shearing, pressure build-up} experienced after drug administration {drug use}.”
Stopping the use of such drugs – on the advice of your doctor – usually solves the problem. Your doctor will work with you to find alternative medications that will be kinder to your system.
Elderly Bed Sores – How to Prevent Bed Sores: Video
Elderly Bed Sores: How to Treat Bed Sores at Home
If your bedsore is at Stage 1, then you can look after it on your own at home, by keeping it clean and dry and by making sure you are keeping pressure off of it.
If the sore has progressed into stage 2 or above, then it is recommended to get it checked out by a nurse or doctor. Always!
Here are a few other treatments you can use on yourself – or the person you are caring for – at home with a Stage 1 bedsore:
• Bed Sore Cream
It is unlikely that an antiseptic or antibiotic cream will be prescribed for a pressure sore. However, a barrier cream for bed sores might be prescribed to make sure there is no further damage done to the affected area.
These barrier creams are formulated to protect the skin from excess moisture that can lead to pressure sores developing.
A good brand is this Cavilon Double Barrier Cream
Or you can ask your local pharmacist about different options, especially if you have any allergies or prone to sensitive skin.
You can also use Vaseline Jelly to seal the pressure sore and can keep it clean and dry by putting a gauze dressing over the top.
• Maalox for Bed Sores
Maalox is a liquid antacid that is prescribed for acid reflux and gastritis.
There is an old-time remedy where you put Maalox onto the affected area, only if it is at stage 1, and leave it to dry in the open air with a light shining on it from about a foot away.
There are people out there that swear by remedies such as these but should be taken with care as they are not medically prescribed.
Before trying any home remedy such as this, check in with your doctor or nurse to make sure it will not cause any more problems.
• How to Use Manuka Honey for Bed Sores
Using manuka honey for bed sores is another old-time remedy.
Honey has been used for thousands of years to treat infected wounds. It has also been researched by medical professionals, in its use in aiding the healing of bedsores in cancer patients. It was found to be useful in the healing process.
It is still wise to be careful when using home remedies on yourself or the person you are caring for. Be mindful to keep the sore clean. Also, be mindful of any allergies that might cause issues with the use of honey.
It is also important to use medical-grade honey such as manuka honey as any other can cause problems with infection, especially raw honey.
If manuka honey has been okayed for use on your bed sores, then begin with clean hands and cleaning the sore with soapy water and drying it gently.
You can then put some honey on to a clean piece of gauze to then be transferred onto the affected area. You can then place a clean, dry dressing, sterile gauze or occlusive dressing over the honey to prevent it from seeping away from the sore.
Replace the bandage as often as needed.
• Can You Use Tea Tree Oil on Bed Sores?
According to Researchgate, Tea tree oil can be used on bedsores, often used by mixing it with other wound-healing or barrier creams.
They concluded that “The tea tree oil can be used successfully in wound healing, due to its good antibacterial and antiseptic activity. It also possesses soothing, cooling, anti-inflammatory properties, which also help to recover the wound.”
However, this is much like Maalox and has very little scientific evidence for the use of tea tree oil on bed sores. It has been used to help wounds that are infected by certain bacteria, but when using it for bed sores specifically, there is still a lot to learn.
As with any other treatment, consult with your doctor and nurse to see what will be the best for your skin and stage of bedsore.
• Treatment for Bed Sores on Buttocks
You should be able to treat bedsores on the buttocks in the same way that you would treat them anywhere else on your body.
The only issue you might have is keeping yourself comfortable while trying to keep pressure off of the sore buttocks. This is where foam cushions or mattresses will come in handy.
The best treatment for bed sores on the buttocks might come in the form of preventative measures. This is because they might be more difficult to heal once formed, and cause such discomfort.
Elderly Bed Sores: Cushions and Beds to Stop Bed Sores
If you suffer from bedsores often – or they lead to any of the later stages – then you might find it useful to look into getting specialised cushions or beds to help prevent the sores.
Pressure-relief cushions for bed sores, as well as mattresses, can help ease pain and discomfort in other parts of your body, such as joint pain, as well as helping your bed sores.
Choosing which type of pressure-relief aid you should use will be specific to your situation. You may wish to read more, in this Bed Sores In-Depth Guide.
Conclusion
Elderly Bed Sores or pressure sores are quite common in elderly people who are also in ill health or have limited mobility. And you spend much of your time sitting or lying down.
They are easily prevented and curable if you catch them quickly. You or your carer should regularly check your skin for signs of pressure damage – especially in awkward areas such as your heels or bottoms.
As much as possible, try to increase your mobility . Suppose you are a carer/ caregiver to an elderly person with partial or total paralysis. In that case, a clock may help you to create an effective turning/ repositioning program.
And be sure to check yourself – or the person you are caring for – daily to ensure you are dealing with bedsores’ symptoms immediately.
Again – very important – If you or your carer notice possible signs of damage, you should immediately tell a healthcare professional.
As you now know, when left too long, these bedsores can become very painful and infected. Which eventually lead to a host of other problems you’re better off without.